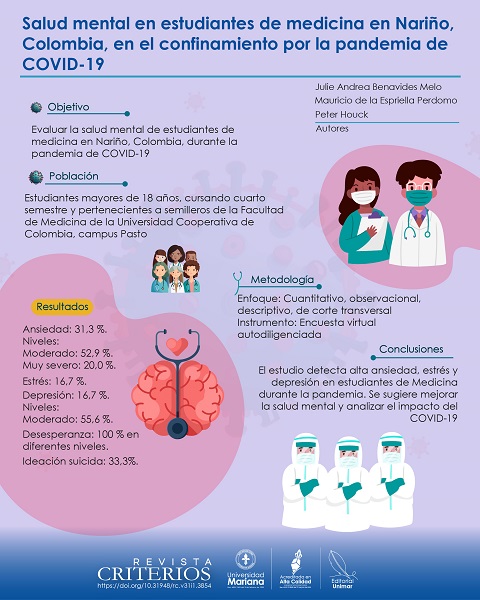
Mental health in medical students in Nariño, Colombia, in the COVID-19 pandemic confinement
DOI:
https://doi.org/10.31948/rc.v31i2.3483Keywords:
coronavirus infections, depression, anxiety, psychological distress, suicidal ideationAbstract
Social distancing, along with other measures to prevent or reduce COVID-19 transmission, had an impact on students’ mental health. Objective: To assess the mental health of medical students in Nariño, Colombia, during the COVID-19 pandemic. Methods: Quantitative, observational, descriptive, cross-sectional, descriptive study. A self-administered virtual survey was administered to students over 18 years of age who were in their fourth semester and belonged to the Faculty of Medicine of the Universidad Cooperativa de Colombia, Pasto campus. The students participated in the study voluntarily, and those who had problems with the Internet connection were excluded. Results: 54 students participated in the survey. Most were 19 years old (33.3%), single (96.3%), belonged to strata 2 to 4 (87.0%), were in their fourth semester (96.0%), and more than half were female (59.0%). A higher prevalence of anxiety (31.3%) was found compared to stress (16.7%) and depression (16.7%). The highest levels of anxiety were moderate (52.9%) and depression (55.6%), while 20.0% of anxiety was very severe. Hopelessness was present at various levels in 100% of the respondents, and 33.3% showed suicidal ideation. Conclusion: It is necessary to implement measures that help to improve and prevent mental health affectations in students, as well as to carry out analytical studies to investigate COVID-19 and its impact on mental health.
Author Biographies
Julie Andrea Benavides Melo, Universidad Cooperativa de Colombia Campus Pasto
Magíster en Epidemiología Clínica, Universidad Cooperativa de Colombia campus Pasto; bióloga. Integrante del grupo de investigación GIISE, San Juan de Pasto, Nariño, Colombia.
Mauricio de la Espriella Perdomo, Universidad Cooperativa de Colombia Campus Pasto
Esp. Psiquiatría, Universidad Cooperativa de Colombia campus Pasto. Integrante del grupo de investigación GIISE, San Juan de Pasto, Nariño, Colombia.
Peter Houck, Universidad de Washington
Esp. Medicina Familiar. Profesor del Departamento de Salud Pública, Universidad de Washington. Seattle, Estados Unidos.
References
Álamo, C., Baader T., Antúnez, S., Bagladi, V., & Bejer, T. (2019). Escala de desesperanza de Beck como instrumento útil para detectar riesgo de suicidio en universitarios chilenos. Revista Chilena de Neuro-psiquiatría, 57(2), 167-75. https://doi.org/10.4067/S0717-92272019000200167 DOI: https://doi.org/10.4067/S0717-92272019000200167
Angela Sweeney, Carol M Worthman, Lucy Yardley, Katherine Cowan, Claire Cope, Matthew Hotopf†, Ed Bullmore (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 7(6):547-560. https://doi.org/10.1016/S2215-0366(20)30168-1
Antony, M., Bieling P., Cox B., Enns M., & Swinson R. (1998). Psychometric properties of the 42 - item and 21 - item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176-181. https://doi.org/10.1037/1040-3590.10.2.176 DOI: https://doi.org/10.1037//1040-3590.10.2.176
Antúnez, Z. y Vinet, E. (2012). Escalas de Depresión, Ansiedad y Estrés (DASS-21): validación de la versión abreviada en estudiantes universitarios chilenos. Terapia Psicológica, 30(3), 49-55. https://doi.org/10.4067/S0718-48082012000300005 DOI: https://doi.org/10.4067/S0718-48082012000300005
Arrieta, K., Díaz, S. y González, F. (2013). Síntomas de depresión, ansiedad y estrés en estudiantes de odontología: prevalencia y factores relacionados. Revista Colombiana de Psiquiatría, 42(2), 173-181. https://doi.org/10.1016/S0034-7450(13)70004-0 DOI: https://doi.org/10.1016/S0034-7450(13)70004-0
Beck, A. T., Weissman, A., Lester, D., & Trexler, L. (1974). The measurement of pessimism: the hopelessness scale. Journal of Consulting and Clinical Psychology, 42(6), 861-865. https://doi.org/10.1037/h0037562 DOI: https://doi.org/10.1037/h0037562
Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., & Zheng, J. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287, 112934. https://doi.org/10.1016/j.psychres.2020.112934 DOI: https://doi.org/10.1016/j.psychres.2020.112934
Castaño, J., Cañón S., Betancur, M., Castellanos, P., Guerrero, J., Gallego, A., & Llanos, C. (2015). Factor de riesgo suicida según dos cuestionarios, y factores asociados en estudiantes de la Universidad Nacional de Colombia sede Manizales. Revista Diversitas, 11(2), 193-205. https://doi.org/10.15332/s1794-9998.2015.0002.02
Denis-Rodríguez, E., Barradas-Alarcón, M., Delgadillo-Castillo, R, Denis-Rodríguez, P. y Melo-Santiesteban, G. (2017). Prevalencia de la ideación suicida en estudiantes de Medicina en Latinoamérica: un meta análisis. Ride, 8(15), 387-418. https://doi.org/10.23913/ride.v8i15.304 DOI: https://doi.org/10.23913/ride.v8i15.304
Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Cohen, R., Everall, I., Ford, T., John, A., Kabir, T., King, K., Madan, I., Michie, S., Przybylski, A., & Shafran, R. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry, 7, 547-560. https://doi.org/10.1016/S2215-0366(20)30168-1 DOI: https://doi.org/10.1016/S2215-0366(20)30168-1
Idrugo, H. y Sánchez, W. (2020). Salud mental en estudiantes de medicina [Carta al editor]. Investigación en Educación Médica, 9(33), 107. https://doi.org/10.22201/facmed.20075057e.2020.33.19215 DOI: https://doi.org/10.22201/facmed.20075057e.2020.33.19215
Jones, E., Mitra, A., & Bhuiyan, A. (2021). Impact of COVID-19 on Mental Health in Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health, 18(5), 2470. https://doi.org/10.3390/ijerph18052470 DOI: https://doi.org/10.3390/ijerph18052470
Kelly, B. D. (2020). Coronavirus disease: challenges for psychiatry. The British Journal of Psychiatry, 217(1), 352-353. https://doi.org/10.1192/bjp.2020.86 DOI: https://doi.org/10.1192/bjp.2020.86
Lee, J. (2020). Mental health effects of school closures during COVID-19. The Lancet. Child & Adolescent Health, 4(1), 421. https://doi.org/10.1016/S2352-4642(20)30109-7 DOI: https://doi.org/10.1016/S2352-4642(20)30109-7
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behaviour Research and Therapy, 33(3), 335-343. https://doi.org/10.1016/0005-7967(94)00075-U DOI: https://doi.org/10.1016/0005-7967(94)00075-U
Lozano-Vargas A. (2020). Impacto de la epidemia del Coronavirus (COVID-19) en la salud mental del personal de salud y en la población general de China. Revista de Neuropsiquiatría, 83(1), 51-56. https://doi.org/10.20453/rnp.v83i1.3687 DOI: https://doi.org/10.20453/rnp.v83i1.3687
Ministerio de Salud y Protección Social. (2020, 28 de marzo). Todos a cuidar nuestra salud mental durante la COVID-19. Boletín de Prensa, (105). https://www.minsalud.gov.co/Paginas/Todos-a-cuidar-nuestra-salud-mental-durante-la-COVID-19.aspx
Montenegro, B. y Yumiseva, S. (2016). Aplicación de la escala DASS-21 para valorar depresión, ansiedad y estrés en los profesionales de salud del Hospital de Especialidades Eugenio Espejo en los meses de julio-agosto del 2016 [Tesis de pregrado, Pontificia Universidad Católica del Ecuador]. PUCE. http://repositorio.puce.edu.ec/bitstream/handle/22000/13926/TESIS%20APLICACION%20ESCALA%20DASS_21.pdf?sequence=1&isAllowed=y
Morote-Jayacc, P., Sandoval, K., Moreno-Molina, M., & Taype-Rondan, A. (2020). Estudios de salud mental en estudiantes de Medicina en el contexto de la COVID-19. Revista Colombiana de Psiquiatría, 49(4), 223-224. https://doi.org/10.1016/j.rcp.2020.07.005 DOI: https://doi.org/10.1016/j.rcp.2020.07.005
Organización Mundial de la Salud (OMS). (2021, 17 de noviembre). Salud mental del adolescente. https://www.who.int/es/news-room/fact-sheets/detail/adolescent-mental-health
Organización Mundial de la Salud. (OMS). (2020, 11 de marzo). Director-General's opening remarks at the media briefing on COVID-19. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
Organización Mundial de la Salud. (OMS). (2020a). Coronavirus. https://www.who.int/health-topics/coronavirus#tab=tab_1
Organización Panamericana de la Salud (OPS). (2023, 6 de mayo). Se acaba la emergencia por la pandemia, pero la COVID-19 continúa. https://doi.org/10.26871/killcanasalud.v6i2.1088 DOI: https://doi.org/10.26871/killcanasalud.v6i2.1088
Ozamiz-Etxebarria, N., Dosil-Santamaria, M., Picaza-Gorrochategui, M. y Idoiaga-Mondragon, N. (2020). Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España. Cadernos de Saúde Pública, 36(4), e00054020. https://doi.org/10.1590/0102-311x00054020 DOI: https://doi.org/10.1590/0102-311x00054020
Peng, E. Y., Lee, M. B., Tsai, S. T., Yang, C. C., Morisky, D. E., Tsai, L. T., Yang, C. C., Morisky, D. E., Tsai, L. T., Weng, Y. L., & Yu, S. (2010). Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. Journal of the Formosan Medical Association, 109(7), 524-32. https://doi.org/10.1016/S0929-6646(10)60087-3 DOI: https://doi.org/10.1016/S0929-6646(10)60087-3
Ramírez-Ortiz, J., Castro-Quintero, D., Lerma-Córdoba, C., Yela-Ceballos, F. y Escobar-Córdoba, F. (2020). Consecuencias de la pandemia Covid-19 en la salud mental asociadas al aislamiento social. Revista Colombiana de Anestesiología, 48(4), e930. https://doi.org/10.5554/22562087.e930 DOI: https://doi.org/10.1590/SciELOPreprints.303
Rueda, M. (2018). Depresión en la mujer. Revista Colombiana de Cardiología, 25(1), 59-65. https://doi.org/10.1016/j.rccar.2017.12.007 DOI: https://doi.org/10.1016/j.rccar.2017.12.007
Santabárbara, J. y Bueno, J. (2022). Impacto de COVID-19 en la salud mental de los estudiantes de medicina. Un meta-análisis. Revista Internacional de Humanidades, 15(3), 2-11. https://doi.org/10.37467/revhuman.v11.4244 DOI: https://doi.org/10.37467/revhuman.v11.4244
Vilchez-Cornejo, J., Quiñones-Laveriano, D., Failoc-Rojas, V., Acevedo, T., Larico-Calla, G., Mucching-Toscano, S., Smith Torres-Román, J., Aquino-Núñez, P., Córdova-De la Cruz, J., Huerta-Rosario, A., Espinoza-Amaya, J., Palacios-Vargas, L. y Díaz-Vélez, C. (2016). Salud mental y calidad de sueño en estudiantes de ocho facultades de Medicina Humana del Perú. Revista Chilena de Neuropsiquiatría, 54(4), 272-281. https://doi.org/10.4067/S0717-92272016000400002 DOI: https://doi.org/10.4067/S0717-92272016000400002
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., Bach, N. C., Ho, R., Sharma, V., & Hoe, C. (2020). A Longitudinal Study on the Mental Health of General Population during the COVID-19 Epidemic in China. Brain, Behavior, and Immunity, 87, 40-48. https://doi.org/10.1016/j.bbi.2020.04.028 DOI: https://doi.org/10.1016/j.bbi.2020.04.028
How to Cite
Downloads
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Revista Criterios

This work is licensed under a Creative Commons Attribution 4.0 International License.
Revista Criterios es publicada por la Editorial UNIMAR de la Universidad Mariana bajo los términos de la licencia Creative Commons Reconocimiento 4.0 Internacional (CC BY 4.0)

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |