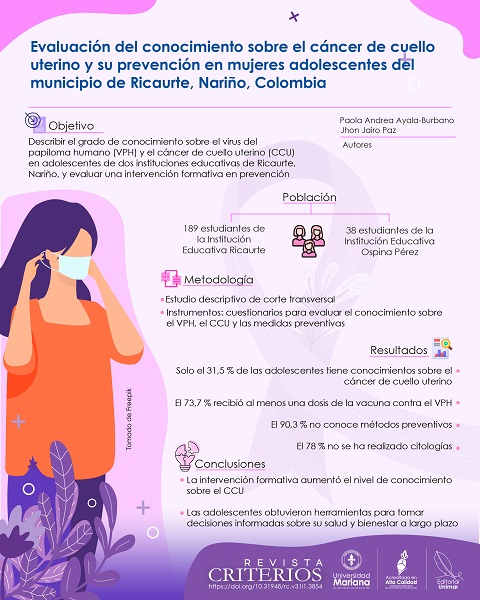
Assessment of knowledge about cervical cancer and its prevention among adolescent women in the municipality of Ricaurte, Nariño, Colombia
DOI:
https://doi.org/10.31948/rc.v31i2.4002Keywords:
human papillomavirus, cervical cancer, adolescents, indigenous population, preventive measuresAbstract
In Colombia, cervical cancer (CC) is the leading cause of death from malignant neoplasms in women. The main causative agent is the human papillomavirus (HPV). The likelihood of developing precancerous lesions at an early stage could increase due to early exposure to risk factors, especially in vulnerable populations such as adolescent girls in the municipality of Ricaurte, Nariño. This study focused on describing the level of knowledge that a group of adolescents from two educational institutions of this municipality have about HPV infection, CC and its relationship with preventive behavior. For this purpose, a formative intervention model was implemented that integrated primary prevention strategies related to the promotion of healthy habits. The results showed that only a minority of the adolescents interviewed were familiar with the CC (31.5%). Early onset of sexual activity was identified as a risk factor for cervical cancer, although a high percentage of adolescents (73.7%) had received at least one dose of HPV vaccine. Regarding preventive measures, 90.3% of the population did not know about any preventive method; 78% had not had a gynecological examination for cytology. The intervention not only increased knowledge about cervical cancer among adolescent girls, but also provided them with the tools to make informed decisions and promote their long-term well-being.
Author Biographies
Jhon Jairo Paz, Universidad Mariana
Tecnólogo en Radiodiagnóstico y Radioterapia. Profesor de Tecnología en Radiodiagnóstico y Radioterapia.
Paola Andrea Ayala-Burbano, Universidad Mariana
Doctora en Ciencias con énfasis en Genética Evolutiva y Biología Molecular; magíster en Genética Evolutiva y Biología Molecular; bióloga. Profesora investigadora de Tecnología en Radiodiagnóstico y Radioterapia.
References
Acevedo-Jiménez, K., Medina Gil, M. y Betancur-Pulgarín, C. L. (2022). Cáncer de Cérvix, una mirada práctica. Revista Médica de Risaralda, 28(2), 151-166. https://doi.org/10.22517/25395203.24936
Aguilar-Pérez, J., Leyva-López, A., Angulo-Nájera, D., Salinas, A. y Lazcano-Ponce, E. (2003). Tamizaje en cáncer cervical: conocimiento dela utilidad y uso de citología cervical en México. Revista Saúde Pública, 37(1), 100-106. https://doi.org/10.1590/S0034-89102003000100015
Alfaro, A. y Fournier, M. (2013). Virus del papiloma humano. Revista Medica de Costa Rica y Centroamerica, LXX(606), 211-217. https://www.binasss.sa.cr/revistas/rmcc/606/art3.pdf
American College of Obstetricians and Gynecologists. (2024). Your first gynecologic visit. https://www.acog.org/womens-health/faqs/your-first-gynecologic-visit#:~:text=When%20should%20I%20have%20my,of%2013%20years%20and%2015
Arams, R., Weinstock, R. E., Satterthwaite Muresianu, E., O'Callaghan, S., Tubridy, E., Torres Maita, Y., & Dolan, S. M. (2021). In the Name of Prevention: Maternal Perspectives on School-Based HPV Vaccination in Rural Southern Chile. Adolescent Health, Medicine and Therapeutics, 12, 27-36. https://doi.org/10.2147/AHMT.S299600
Araújo, A. S. de B., Spindola, T., Sousa, K. S. de, Araújo, A. B. de, & Martins, E. R. C. (2020). Práticas de cuidado com a saúde sexual de jovens universitárias. Revista de Pesquisa, 12, 1215-1220.
Ayala, J. (2014). La salud en Colombia: más cobertura pero menos acceso [Documentos de trabajo sobre economía regional]. Banco de la República, Centro de Estudios Económicos Regionales (CEER) Cartagena. https://www.banrep.gov.co/sites/default/files/publicaciones/archivos/dtser_204.pdf
Bazargan, M., Bazargan, S. H., Farooq, M., & Baker, R. S. (2004). Correlates of cervical cancer screening among underserved Hispanic and African-American women. Preventive Medicine, 39(3), 465-473. https://doi.org/10.1016/j.ypmed.2004.05.003
Benach, J. y Muntaner, C. (2005). Aprender a mirar la salud: cómo la desigualdad social daña nuestra salud. Editorial El Viejo Topo.
Binefa, G., García, M., Peiró, R., Molina-Barceló, A. y Ibáñez, R. (2016). Cómo evaluar y reducir desigualdades sociales en los programas de cribado de cáncer. Gaceta Sanitaria, 30(3), 232-234. https://doi.org/10.1016/j.gaceta.2016.01.008
Bosch, F. X., Burchell, A. N., Schiffman, M., Giuliano, A. R., de Sanjose, S., Bruni, L., Tortolero-Luna, G., Kjaer, S. K., & Muñoz, N. (2008). Epidemiology and Natural History of Human Papillomavirus Infections and Type-Specific Implications in Cervical Neoplasia. Vaccine, 26(10), k1-k16. https://doi.org/10.1016/j.vaccine.2008.05.064
Bratwaite, C., González, I., Campo, Z. y De León, R. (2002). Diagnóstico del virus de papiloma humano por papanicolau y PCR en un grupo de adolescentes y mujeres jovenes. Pesquisa Panamá, 6, 1-6. https://pesquisa.bvsalud.org/portal/resource/pt/lil-471955
Buskwofie, A., David-West, G., & Clare, C. A. (2020). A Review of Cervical Cancer: Incidence and Disparities. Journal of the National Medical Association, 112(2), 229-232. https://doi.org/10.1016/j.jnma.2020.03.002
Castro, E., Miranda, P. y Borre, O. (2012). Conocimientos, Actitudes Y Prácticas Acerca Del Virus Del Papiloma Humano En Adolescentes Escolarizados. Revista Ciencias Biomédicas, 3(2), 275-281. https://revistas.unicartagena.edu.co/index.php/cbiomedicas/issue/view/210
Cordoba-Sanchez, V., Lemos, M., Tamayo-lopera, D. A., & Gorin, S. S. (2022). HPV-Vaccine Hesitancy in Colombia : A Mixed-Methods Study. Vaccines, 10, 1-16. https://doi.org/10.3390/vaccines10081187
Davies-Oliveira, J. C., Smith, M. A., Grover, S., Canfell, K., & Crosbie, E. J. (2021). Eliminating cervical cancer: progress and challenges for high-income countries. Clinical Oncology, 33(9), 550-559. https://doi.org/10.1016/j.clon.2021.06.013
Fica, A. (2014). Prevención del cáncer cérvico-uterino en Chile. Mucha vacuna y poco Papanicolau. Revista Chilena de Infectologia, 31(2), 196-203. https://doi.org/10.4067/S0716-10182014000200010
Gobernación de Nariño. (2024). Plan de Desarrollo Departamental 2024-2027. Nariño.
Hardon, A., Pell, C., Taqueban, E., & Narasimhan, M. (2019). Sexual and reproductive self care among women and girls: Insights from ethnographic studies. BMJ (Online), 365, 1-4. https://doi.org/10.1136/bmj.l1333
Iova, C. F., Badau, D., Daina, L. G., Daina, M. D., & Șuteu, C. L. (2023). Evaluation of the Knowledge and Attitude of Adolescents Regarding the HPV Infection, HPV Vaccination and Cervical Cancer in a Region from the Northwest of Romania. Patient Preference and Adherence, 17, 2249-2262. https://doi.org/10.2147/PPA.S421875
Krakauer, E. L., Kwete, X., Kane, K., Afshan, G., Bazzett-Matabele, L., Bien-Aimé, D. D. R., Byrne-Martelli, S., Connor, S., Correa, R., Devi, C. R. B., Diop, M., Gafer, N., Goodman, A., Grover, S., Hasenburg, A., Irwin, K., Thanh Khanh, Q., Kumar, S., Nevzorova, D., … Fidarova, E. (2021). Cervical Cancer-Associated Suffering: Estimating the Palliative Care Needs of a Highly Vulnerable Population. JCO Global Oncology, 7, 862-872. https://doi.org/10.1200/GO.21.00025
Kjaer, S. K., Chackerian, B., van den Brule, A. J., Svare, E. I., Paull, G., Walbomers, J. M., Schiller, J. T., Bock, J. E., Sherman, M. E., Lowy, D. R., & Meijer, C. L. (2001). High-risk human papillomavirus is sexually transmitted: evidence from a follow-up study of virgins starting sexual activity (intercourse). Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 10(2), 101-106. https://pubmed.ncbi.nlm.nih.gov/11219765/
Mathew, A., George, P. S., Ramadas, K., Mathew, B. S., Kumar, A., Roshni, S., Lalithamma Jayakumar, K. N., & Booth, C. M. (2019). Sociodemographic factors and stage of cancer at diagnosis: A population-based study in South India. Journal of Global Oncology, 2019(5), 1-10. https://doi.org/10.1200/JGO.18.00160
Mendoza, L., Arias, M., Pedroza, M., Micolta, P., Ramírez, A., Cáceres, C., López, D., Núñez, A. y Acuña, M. (2012). Actividad sexual en adolescencia temprana: problemade salud pública en una ciudad colombiana. Revista Chilena de Obstricia y Ginecología, 77(4), 271-279. https://doi.org/10.4067/S0717-75262012000400006
Mesa-Arango, J. A., Tapia-Vela, L. J., Loaiza-Díaz, N., Echeverry-Chica, J. y Toro-Montoya, A. I. (2021). Detección y genotipificación del virus del papiloma humano de alto riesgo mediante PCR multiplex en tiempo real (RT-PCR VPH AR). Medicina y Laboratorio, 25(2), 547-550. https://doi.org/10.36384/01232576.439
Ministerio de Salud y Protección Social. (2017). Lineamientos. Incorporación del enfoque intercultural en los procesos de formación de talento humano en salud, para el cuidado de la salud de pueblos indígenas en Colombia. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/TH/Incorporacion-enfoque-intercultural-formacion-ths-pueblos-indígenas.pdf
Ministerio de Salud. (2024, 19 de julio). Lineamientos técnicos y operativos para la vacunación contra el virus del papiloma humano. Alcance en el marco de la estrategia "Colombia sin cáncer de cuello uterino". Vacunación contra el VPH niñas de 9 a 17 años y niños de 9 a 14 años. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/PAI/lineamientos-vacunacion-contra-virus-papiloma-humano-ninas-ninos.pdf
Moeinzadeh, M., Kheirkhah, B., Amini, K., & Pouryasin, A. (2020). Classification and identification of human papillomavirus based on its prevalence and development of cervical lesion among Iranian women. BioImpacts, 10(4), 235-242. https://doi.org/10.34172/bi.2020.30
Muñoz, N., & Bravo, L. E. (2012). Epidemiology of cervical cancer in Colombia. Colombia Médica, 43(4), 298-04. https://doi.org/10.25100/cm.v43i4.1269
Murfin, J., Irvine, F., Meechan-Rogers, R., & Swift, A. (2020). Education, income and occupation and their influence on the uptake of cervical cancer prevention strategies: A systematic review. Journal of Clinical Nursing, 29(3-4), 393-415. https://doi.org/10.1111/jocn.15094
Narasimhamurthy, M., & Kafle, S. U. (2022). Cervical cancer in Nepal: Current screening strategies and challenges. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.980899
Organización Mundial de la Salud (OMS). (2024, 5 de marzo). Cáncer de cuello uterino. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer?gad_source=1&gclid=CjwKCAjwufq2BhAmEiwAnZqw8kOCK5P1q_mx8VUDhANVBXc_84Od_UhG59eSobbRQjBVDCR24eqvVhoCoWsQAvD_BwE
Osorio-Castaño, J. H., Pérez-Villa, M., Montoya-Zapata, C. P., & Cardona-Restrepo, F. A. (2020). Características citológicas previas al diagnóstico de cáncer de cérvix en mujeres de Medellín (Colombia). Universidad y Salud, 22(3), 231-237. https://doi.org/10.22267/rus.202203.195
Ospina M. (2015). Observatorio Nacional de Cáncer Colombia. Revista Facultad Nacional de Salud Pública, 33(2), 262-276. https://doi.org/10.17533/udea.rfnsp.v33n2a13
Owusu, G. A., Eve, S. B., Cready, C. M., Koelln, K., Trevino, F., Urrutia-Rojas, X., & Baumer, J. (2005). Race and ethnic disparities in cervical cancer screening in a safety-net system. Maternal and Child Health Journal, 9(3), 285-295. https://doi.org/10.1007/s10995-005-0004-8
Qin, T., Li, S., Henry, L. E., Liu, S., & Sartor, M. A. (2021). Molecular tumor subtypes of hpv‐positive head and neck cancers: Biological characteristics and implications for clinical outcomes. Cancers, 13(11), 1-21. https://doi.org/10.3390/cancers13112721
Shew, M. L., Fortenberry, J. D., Tu, W., Juliar, B. E., Batteiger, B. E., Qadadri, B., & Brown, D. R. (2006). Association of condom use, sexual behaviors, and sexually transmitted infections with the duration of genital human papillomavirus infection among adolescent women. Archives of Pediatrics & Adolescent Medicine, 160(2), 151-156. https://doi.org/10.1001/archpedi.160.2.151
Shin, H. Y., Song, S. Y., Jun, J. K., Kim, K. Y., & Kang, P. (2021). Barriers and strategies for cervical cancer screening: What do female university students know and want? PLoS ONE, 16(10), 1-12. https://doi.org/10.1371/journal.pone.0257529
Sivaranjini, K., Oak, A., Cheulkar, S., Maheshwari, A., Mahantshetty, U., & Dikshit, R. (2023). Role of Education and Income on Disparities of Time‑to‑Treatment Initiation and its Impact on Cervical Cancer Survival. Indian Journal of Public Health, 67(2), 235-239. https://doi.org/10.4103/ijph.ijph_1299_22
Solano-Dazzarola, P., Grilló, G., López, J. y Montoya-Cobo, E. (2023). Panorama colombiano del cáncer de mama, cérvix y próstata. Revista Salutem Scientia Spiritus, 9(1), 28-35. https://orcid.org/0000-0002-9557-6621
Stelzle, D., Tanaka, L. F., Lee, K. K., Ibrahim Khalil, A., Baussano, I., Shah, A. S. V., McAllister, D. A., Gottlieb, S. L., Klug, S. J., Winkler, A. S., Bray, F., Baggaley, R., Clifford, G. M., Broutet, N., & Dalal, S. (2021). Estimates of the global burden of cervical cancer associated with HIV. The Lancet Global Health, 9(2), e161-e169. https://doi.org/10.1016/S2214-109X(20)30459-9
Swatzyna, R. J., & Pillai, V. K. (2013). The effects of disaster on women's reproductive health in developing countries. Global Journal of Health Science, 5(4), 106-113. https://doi.org/10.5539/gjhs.v5n4p106
Tao, X., Zhang, H., Wang, S., Chen, T., Cong, Q., Wang, L., Zhou, X., & Zhao, C. (2021). Prevalence and carcinogenic risk of high-risk human papillomavirus subtypes in different cervical cytology: a study of 124,251 cases from the largest academic center in China. Journal of the American Society of Cytopathology, 10(4), 391-398. https://doi.org/10.1016/j.jasc.2021.03.006
Urrutia, M., Concha, X., Riquelme, G. & Padilla, O. (2012). Conocimientos y conductas preventivas sobre cáncercérvico-uterino y virus papiloma humano en un grupode adolescentes chilenas. Revista Chilena de Infectología, 29(6), 600-607. https://doi.org/10.4067/S0716-10182012000700003
Vale, D. B., Teixeira, J. C., Bragança, J. F., Derchain, S., Sarian, L. O., & Zeferino, L. C. (2021). Elimination of cervical cancer in low- and middle-income countries: Inequality of access and fragile healthcare systems. International Journal of Gynecology and Obstetrics, 152(1), 7-11. https://doi.org/10.1002/ijgo.13458
Vallone, F., Lemmo, D., Martino, M. L., Donizzetti, A. R., Freda, M. F., Palumbo, F., Lorenzo, E., D'Argenzio, A., & Caso, D. (2022). Factors promoting breast, cervical and colorectal cancer screenings participation: A systematic review. Psycho-Oncology, 31(9), 1435-1447. https://doi.org/10.1002/pon.5997
Winer, R. L., Lee, S. K., Hughes, J. P., Adam, D. E., Kiviat, N. B., & Koutsky, L. A. (2003). Genital human papillomavirus infection: Incidence and risk factors in a cohort of female university students. American Journal of Epidemiology, 157(3), 218-226. https://doi.org/10.1093/aje/kwf180
Yamaguchi, M., Sekine, M., Hanley, S. J. B., Kudo, R., Hara, M., Adachi, S., Ueda, Y., Miyagi, E., & Enomoto, T. (2021). Risk factors for HPV infection and high-grade cervical disease in sexually active Japanese women. Scientific Reports, 11(1), 1-9. https://doi.org/10.1038/s41598-021-82354-6
Yazdani, F., Simbar, M., Hamzehgardeshi, Z., Zare, E., & Nasiri, M. (2023). Explaining sexual self-care status and its predictor factors in women referring to healthcare centers of Sari, Iran, 2021. BMC Women's Health, 23(1), 1-12. https://doi.org/10.1186/s12905-023-02196-4
Yépez Chamorro, M. C., Bravo Goyes, L. M., Jurado Fajardo, D., Mena Huertas, J., & Casas, H. M. (2022). Incidence and mortality by cancer in the Pasto municipality, Colombia. 2013-2017. Colombia Medica, 53(1), e2054952. https://doi.org/10.25100/cm.v53i1.4952
Zhang, M., Sit, J. W. H., Chan, D. N. S., Akingbade, O., & Chan, C. W. H. (2022). Educational Interventions to Promote Cervical Cancer Screening among Rural Populations: A Systematic Review. International Journal of Environmental Research and Public Health, 19(11), 68-74. https://doi.org/10.3390/ijerph19116874
Zhou, Y., Shi, X., Liu, J., & Zhang, L. (2023). Correlation between human papillomavirus viral load and cervical lesions classification: A review of current research. Frontiers in Medicine, 10, 1-6. https://doi.org/10.3389/fmed.2023.1111269
How to Cite
Downloads
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Revista Criterios

This work is licensed under a Creative Commons Attribution 4.0 International License.
Revista Criterios es publicada por la Editorial UNIMAR de la Universidad Mariana bajo los términos de la licencia Creative Commons Reconocimiento 4.0 Internacional (CC BY 4.0)

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |